myasthenia gravis ( symptoms, couses treatment )
What is myasthenia gravis, and is there any cure?
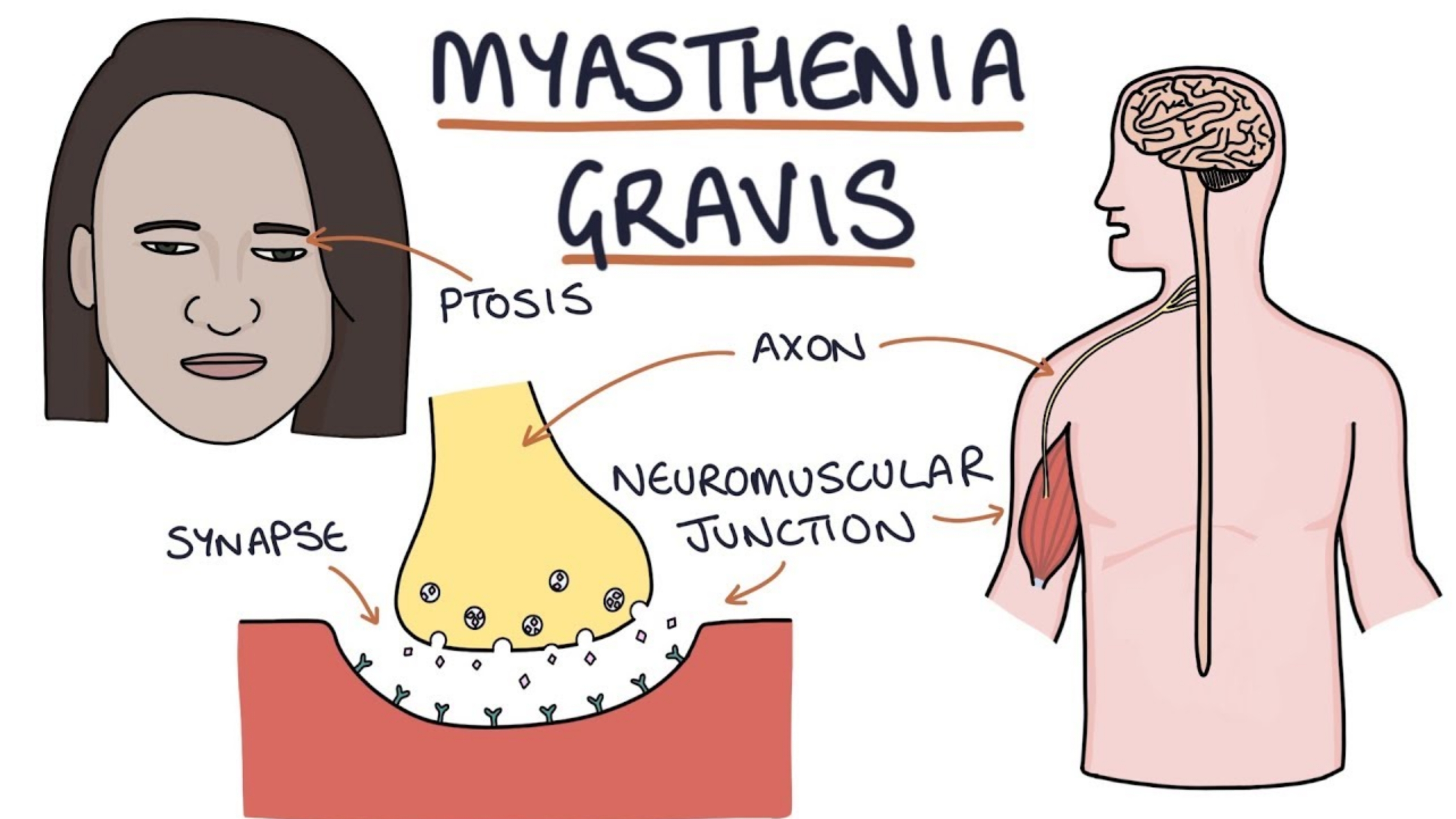
MG is a somewhat rare condition of the neuro-muscular junction (NMJ). The NMJ is a complex structure, where the nerve ends on the muscle, and nerve impulses are transmitted across a small ‘gap’, which then initiates the process of muscle contraction. Each muscle fiber has several
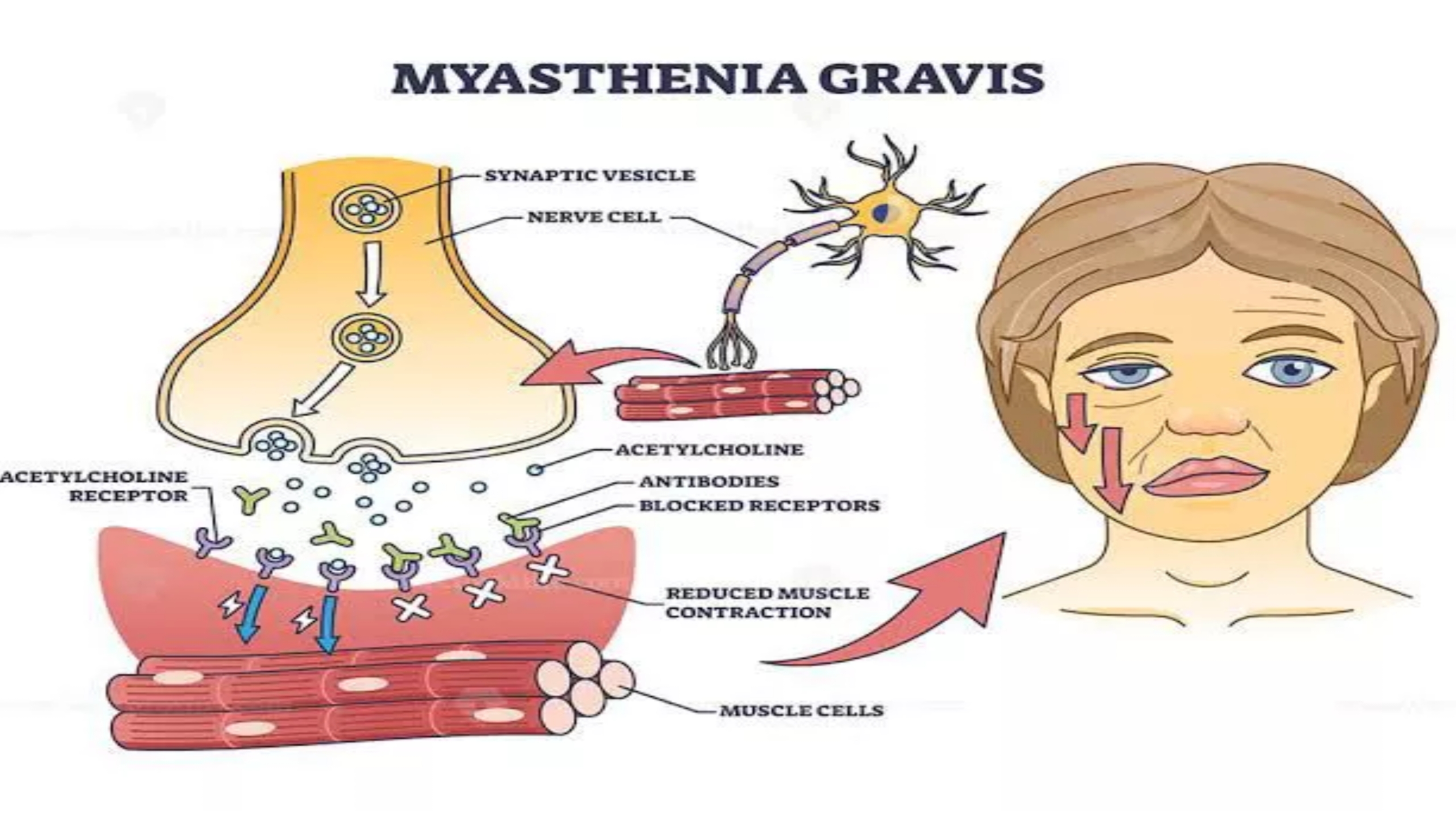
nerve fibrils ending on it, and each of these have an NMJ, and each NMJ has a receptor on the muscle - end of the gap where the transmitter from the nerve end attaches to transfer the ‘information’. In the variety of MG which is the most common, there is an autoimmune process causing damage to these receptors. Specifically, antibodies to this receptor, which is actually the receptor for the principle neurotransmitter for nerve-muscle (skeletal muscle) interaction, called ACETYL-CHOLINE.
So, basically, in MG, there are antibodies to the NICOTINIC-form of the Acetylcholine receptor; depending on the disease activity, there is a variable degree of damage - not only loss of the receptor (in terms of reduced numbers of receptors available for ACH to connect with) but also other damage of the muscle surface - which over a period of time can become irreversible, since new ACH-receptor cannot be synthesized or positioned.
This then is the CORE abnormality in MG; there are many more details and ramifications, but understanding this should help to understand the CORE symptom in MG - which is FATIGUABILITY.
The individual with MG is able to initiate muscle contractions, but due to deficiency of Ach-receptors, there is a reduced strength of the contractions, and the effect wears off fast, so repeated actions produce less strong contractions. If the same group of muscles are made to contract for more than a few times in quick succession, the sufferer may not be able to initiated the movement at all; after a period of rest, some strength may be restored - and this is the reason why sufferers of MG have this peculiar symptom - eye lids drooping after a while, then returning back to normal; able to swallow the first few mouthfuls, then becoming unable to swallow - and so on.
It is a devastating illness because ultimately respiratory muscles get affected, and that can lead to death.
The good part is that MG can be cured - under certain conditions. 30% of patients remit in the first year, but many of these have a recurrence in a few years. Another 30% will remit within 3 years. The last 30% don’t undergo spontaneous remission - in these patients, an extensive search for a thymic gland abnormality is made, and if a tumor is found, then they may go for early thymic removal with potential cure. Among those who have a normal thymus, removal can give a high rate of cure. But I have personally had patients who had recurrence even after successful remission following thymectomy - so it is very variable, and genetics has a strong role to play there. There is a lot of detail in all this, and enough cannot be shared in a message like this.
Is there a blood test to diagnose Myasthenia Gravis, and what is the marker for it within the blood?
Most common antibody is the detection of antibodies against the acetylcholine receptor - positive in 50% of ocular MG (only symptoms and signs in the eyes - droopy eyelids and double vision) and 85% of generalized (may have ocular but also have weakness of face, speech and swallowing, breathing, neck, arms and legs to varying degrees) MG. This antibody test is pretty much routinely available in most westernized countries, I am not sure about how available it is outside ‘westernized’ countries.
The rate of positive anti-MuSK antibodies varies geographically (higher in areas with more non-Caucasians) but they are positive in 0–10% of generalized, very rare in ocular MG.
Other antibodies more recently discovered include clustered AChR, clustered MuSK (clustered means a different way of detecting these antibodies, using a cell based assay rather than a soluble AChR radioimmunoassay or ELISA), LRP4, agrin or cortactin.
Their rate of positivity and role in the diagnosis of MG is less certain at present but most (perhaps with the exception of LRP4) are also highly specific for MG. Specific means that if you have these antibodies positive, you almost certainly have MG (some patients with a thymoma may have positive AChR but no clinical evidence for MG - yet). LRP4 has been found to be positive in other neurological disease like ALS so it is less specific for MG.
Positive serology (antibody testing) is the MOST useful diagnostic test as most are very specific for MG (99.9% for AChR) and help guide management in some areas. So, responses to some medications and not to others may vary depending on whether AChR or MuSK antibodies are positive. The risk of having an underlying tumour of the thymus [thymoma] is pretty much exclusive to patients with positive AChR antibodies and is very rare with others.
The benefit of doing a thymectomy in early onset (onset less than 50 years of age, some use 60 or even 65) AChR antibody positive MG when there isn’t a thymoma, usually hoping to find a ‘hyperplastic thymus’, is mostly associated with positive AChR antibodies. Although perhaps a bit controversial to some, the thymus in patients with positive MuSK antibodies is almost always normal and no different from healthy individuals so most neurologists managing MG would not consider suggesting a thymectomy if MuSK antibodies are positive.
Removing a hyperplastic thymus (you can't tell whether it will be until it is removed) helps many patients with AChR antibody positive MG so that they do better and require lower doses of drugs like prednisone and azathioprine. The removal of a thymoma, although almost always necessary to get rid of a tumour which initally is small and benign in most, doesn’t usually help the course of the MG.














Post a Comment